Eastern Colorado, like most of rural middle America, is flyover country, recognized only by the corn circles of center-pivot irrigation, the smells of confined cattle operations, or the small concentrations of lights at night seen from 30,000 feet. Many think of this as the last place on earth to live. But this place also has tremendous strengths and assets, including a willingness to come together to find solutions and a desire to always learn more. The people of rural Colorado are resourceful and curious—curious how to make corn grow with less water, how to breed cattle with the best lean-to-fat ratio, and how to live healthier lives with fewer health care resources.
The High Plains Research Network Community Advisory Council is one example of this curiosity, desire to learn, and pursuit for ways to help their communities. The High Plains Research Network (HPRN), established in 1997 and housed at the University of Colorado Denver Department of Family Medicine, is an integrated network of 54 primary-care practices, 16 hospitals, 150 providers, and the communities in all 16 counties of eastern rural and frontier Colorado. The network covers over 30,000 square miles and includes approximately 150,000 Coloradoans, 30 percent of whom are Hispanic. The HPRN is guided by the Community Advisory Council (C.A.C.), a group of local farmers, ranchers, teachers, students, small business folks, and retirees. This group is critical to ensuring that the work of the HPRN meets the communities’ needs.
Several years ago, the HPRN C.A.C. identified mental health as a priority health issue. Members experienced loss of youth and elderly farmers to suicide, the frustration of seeing loved ones develop and suffer from severe mental health conditions, and the slow toll of dysthymia (mild but chronic depression) and increased anxiety. Research also says residents in eastern Colorado have worse mental health outcomes: In the HPRN region, the average number of days of poor physical or mental health experienced by adults that kept them from performing their usual activities is higher than for the rest of the state.1 Proportionately, fewer physicians and psychologists are available in eastern Colorado than the rest of Colorado. Fifteen of the 16 counties the HPRN clinics serve are officially designated Health Professional Shortage Areas (meaning there is a shortage of primary care and mental health care), and 12 counties are Medically Underserved Areas (too few primary care providers, high infant mortality, high poverty, or a high elderly population).2 This combination of data and lived experience launched mental health to the top of the C.A.C.’s list of health issues needing urgent attention and seriously committed, creative, and multidisciplinary people.
The “community of solution” concept was first introduced in the 1966 Folsom Report and recognizes the critical links between communities, public health, and primary care.3 Communities of solution move beyond jurisdictional boundaries and promote community-led initiatives that improve population health.4 This article describes how a unique participatory collaboration between the residents, primary care practices, and practice-based researchers at the University of Colorado has led to a community of solution working to address mental, emotional, and behavioral health needs in eastern Colorado.
Community-Based Approaches for Supporting Rural Mental Health
Like any avid farmer or rancher, the HPRN C.A.C. recognized the need to become more educated and learn as much as possible about this broad field of mental health to help it determine what could be done. Propelled by this interest and supported by the University of Colorado Department of Family Medicine, the HPRN embarked on a multiyear endeavor to identify and improve access to mental health services and prevent mental, emotional, and behavioral health problems. The C.A.C. met with five different experts in the field over 18 months to learn about major mental illnesses, policy issues, and integrated behavioral health care (the practice of integrating behavioral health services into primary care). Members learned about the broad scope of mental health issues; they also delved into narrower topics of suicide prevention, substance use disorder, prevention in early childhood, and Mental Health First Aid, a course on responding to signs of mental illnesses, substance use disorders, and crisis situations. After much discussion and contemplation of what they could and could not impact, the community members decided not to focus on one particular condition (like depression) or even one particular group of people (like older, male farmers, who have the region’s highest suicide rates). Instead, they were driven to address the broad range of the community’s mental, emotional, and behavioral health needs. Extensive community research identified unexpected opportunities for helping people recognize early precursors and prevent mental, emotional, and behavioral health problems.
The COMET Program
A local young man was tending bar in small-town Colorado. On a July afternoon, one of his customers was a guy from a harvest crew traveling through, following the wheat crop from Texas to North Dakota. As the bartender worked, he learned that the patron was despondent, depressed, and suicidal. The young bartender had no knowledge of what to do, what to say, or how to help.
A major process the HPRN C.A.C. sought to improve was the path people could take to access mental health care and support. However, they and HPRN leadership could not identify guidelines around this specific step, especially information that resonated with their communities. The group turned to the method of appreciative inquiry (AI)—an exploration of the strengths and opportunities that exist within an organization or network. It wanted to hear directly from local residents about successful steps they had taken to obtain, or to help provide others with, various forms of mental, emotional, and behavioral health support and care.
Back to the young man. He became a member of the HPRN C.A.C. Over time, he went on to college to study aeronautical engineering. Data obtained through the AI method revealed to him and the rest of the group that many of these elements of successful solutions took place in the community—outside of hospitals, clinics, or therapists’ offices. Places for initiating mental health support and providing services might be the golf course, one’s own home, a parking lot, or the hardware store. These conversations might be with a friend, an acquaintance, or just someone who noticed something was not quite right. In many cases, the conversation was not with someone closest to the person in need. Through AI, the C.A.C. discovered the important role this “other person” plays in prompting a conversation about mental health—and that almost anyone can be this person. The C.A.C. was challenged to be that “other person,” and in turn wanted to challenge its communities to do the same when the opportunity arose.
The C.A.C. created a visual for what the AI data had revealed, illustrating the role of this “other person” impacting the trajectory of mental illness (see Figure 1). Looking at the diagram, the young engineer declared that this is exactly how NASA launches spaceships and rovers into deep space. The Mars Rover was not shot up directly toward Mars. Instead, it used “gravity assist” to first head toward the moon and then used the moon’s gravity to slingshot around the moon, dramatically changing its trajectory and sending it along a new path toward its destination—Mars. Similarly, the “other person” alters another’s path away from crisis and toward recovery and health. Changing Our Mental and Emotional Trajectory (COMET) activates people to become the “other person.” This intervention can alter the vulnerable person’s trajectory, build resilience, and encourage professional care. The approach supports fellow community members to experience fewer and less severe mental, emotional, and behavioral health problems.
Figure 1
Trajectory of Mental Illness
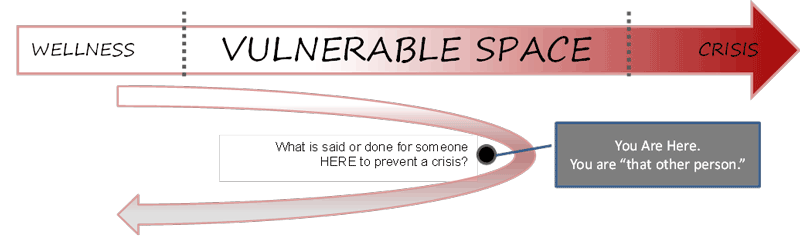
Being the “other person” does not require technical mental health language. Rather, this crucial shift requires being prepared to initiate a conversation. The C.A.C. was acutely aware that many people feel inadequately prepared to respond to someone’s mental, emotional, or behavioral health problem, despite a desire to help. Having learned of the Patient Health Questionnaire (PHQ) used in clinical settings, the C.A.C. created a natural, five-question conversation guide that could be used by anyone to be the “other person.” These became the Conversational Gravity Assist (see Figure 2).
Figure 2
Conversational Gravity Assist
- “How are you? No really, how are you?”
- “You don’t seem like yourself.”
- Observation of mood or behavior. (“I haven’t seen you at bowling for a few months” or “You seem down.”)
- Question about family or social life. (“How are things at home/work/school?”)
- Invitation to engage. (“Would you like to talk about it?”)
Imagine that while walking to your car after work, you see a coworker who has not quite been herself recently. The standard, “How are you?” is not enough, so you include the second half of that question: “How are you really?” Second, you add an observation that you have made about her mood or behavior. “I noticed you weren’t at the football game last week; is everything going OK?” Or you might ask a question about family or social life: “I know John just went to college; how are you doing with that?” Now, you may have an opportunity to invite the person to engage by sharing with her that you have gone through something similar and by talking about how you overcame it. You might think that you have no idea how to help this person, but you do know a therapist who works at the local integrated primary care clinic. Or you might want to talk more later and invite the person to grab coffee with you this week and continue chatting. The Conversational Gravity Assist is designed to be flexible so that it can be used by any “other person” in any safe venue. It includes several suggested questions for each item (1‒5). COMET uses the Conversational Gravity Assist to help community members build resilience, seek professional care, and live with fewer and less severe mental, emotional, and behavioral health problems. COMET is powerful because it uses evidence-based programs and techniques, along with strong community engagement. It gives people permission to ask, be asked, lean in to a possible mental health situation with easy and natural questions, and strengthen the community fabric.
IT MATTTRs™ Colorado
The HPRN staff regularly visit the practices and communities across eastern Colorado. Each of the 55 primary care practices has its own unique culture—from the small house clinic to the new 10-exam-room clinic. Some clinics are next door to the hospital; others are 40 miles from the closest health care facility. In the early 2010s, HPRN began hearing about the problem with narcotics. The typical story was of the 50-year-old patient with recurrent knee pain who had surgery in the city and came back to the rural clinic a month later for more Percocet. The clinics did not have adequate treatment for this new wave of opioid use disorder (OUD). Simply not writing another prescription too often led patients to find opioids elsewhere, including low-cost, black-tar heroin. People were dying from opioid overdoses. The network leaders heard this refrain over and over. When the Agency for Health Research and Quality released a grant application to increase rural primary care practices’ capacity to treat OUD, the HPRN submitted a full-throated proposal for rural Colorado and was one of five entities in the country to receive funding for this innovative work.
The HRPN C.A.C. immediately engaged in the project. To get the project started, the C.A.C. used the Boot Camp Translation process5, 6 to translate the complex medical jargon used in evidence-based guidelines by the Centers for Disease Control and the Substance Abuse and Mental Health Services Administration into understandable, actionable messages and creative materials to change the conversation around OUD and medication-assisted treatment in their communities. The language they used to discuss the issue set the tone for a practice-based curriculum for their local primary care providers and behavioral health providers. Implementation of Technology Medication Assisted Treatment Team Training for Rural Colorado (IT MATTTRs™ Colorado) was taking shape.
Led by the community-academic partnership, IT MATTTRs™ Colorado includes: 1) support for physicians, nurse practitioners, and physician assistants to receive formal Drug Enforcement Administration (DEA) training on the use of buprenorphine for medication-assisted treatment of opioid dependency and waiver to prescribe; 2) onsite training for the whole primary care practice (providers and staff) in team-based care for their patients suffering from OUD, calling out the fact that everyone in the practice has a role—front-desk staff, nurses, medical assistants, prescribers, administrators, and billing staff; and 3) community education and action intervention to increase awareness, inform community members, and provoke action to support and enhance the impact of the new resources becoming available in practices. This includes using the language and communication tools developed with the Boot Camp Translation process, such as drink coasters in bars and restaurants; a series of posters; inserts for church bulletins and sports programs; pharmacy bags; library bookmarks; movie theater trailers; and stories in local newspapers (see Figure 3).
Figure 3
IT MATTTRs™ “Have You Met MAT?” Community Education and Action Intervention Materials
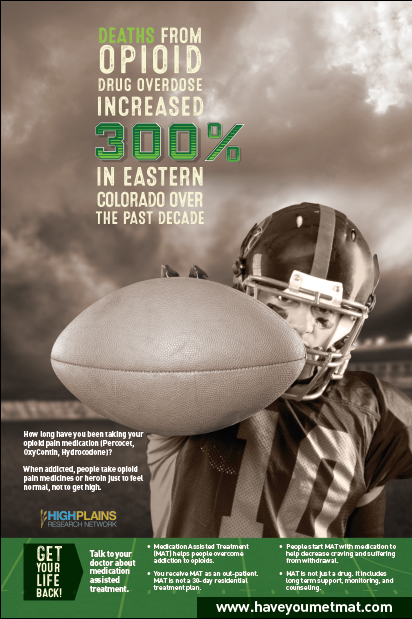
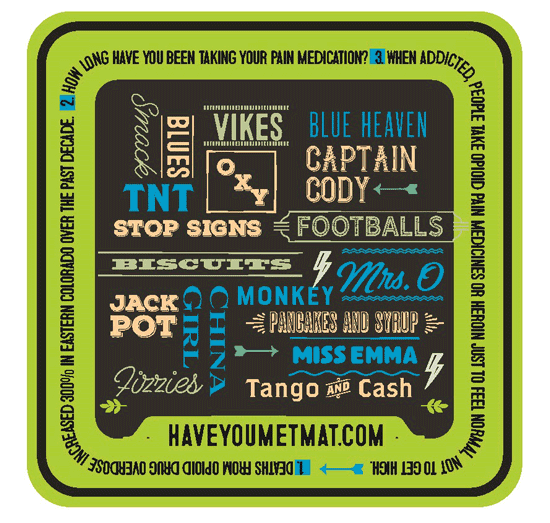

Communities and practices responded. Almost 30 providers have completed training in prescribing buprenorphine for OUD, and 16 received their waiver from the DEA to prescribe buprenorphine for OUD. Over 20 practices signed up for the IT MATTTRsTM team training and practice support to deliver medication-assisted treatment for OUD. The C.A.C. delivered materials to local restaurants, bars, churches, community organizations, pharmacies, and schools. While the implementation and evaluation work in eastern Colorado continues, other practices and organizations in the state and around the country have heard about the IT MATTTRs™ program. With additional state and federal funding, IT MATTTRsTM has expanded throughout Colorado, including training 45 additional practice facilitators to deliver the curriculum to 70 additional primary care practices in rural and urban communities. Additionally, groups in Montana, North Carolina, and California are preparing for IT MATTTRsTM curriculum trainings and exploring the “Have You Met MAT?” community intervention. Rural communities working together can build a local community of solution that just might be a solution in other places as well.
UPSTREAM! Together and the MEB Box™ Program
UPSTREAM! Together aims to prevent mental, emotional, and behavioral health problems through a community-based participatory approach. The HPRN is one of three UPSTREAM! Together pioneer communities. With 20 years of experience on the high plains of Colorado, extensive community relationships, and deep local knowledge and expertise, HPRN led the exploration of how northeast Colorado can move forward to prevent mental, emotional, and behavioral problems by focusing on youth. Over an eight-month period, the HPRN UPSTREAM! Together Community Council, comprised of C.A.C. and other community experts, completed a rigorous Boot Camp Translation. It established a shared understanding of the science underlying the prevention of mental, emotional, and behavioral (MEB) health problems, settled on MEB as a usable acronym to help normalize discussion about its health aspirations, and prioritized a focus and strategy for prevention. The result was the MEB Box™ Program.
The MEB Box™ Program aims to create a culture where MEB health is woven into the community fabric as part of conversations, public health and clinical care, school life, city and county funding, and organizational and public policy. Specifically, the MEB Box™ Program takes a universal prevention approach to support and enhance positive relationships through social connections and prosocial behaviors, teach emotional regulation, and support and encourage early cognitive development. The goal is to provide children and their caregivers with tools, resources, and supports so that every child may reach adulthood unencumbered by mental, emotional, and behavioral health problems.
The MEB Box™ Program includes an actual physical box delivered to children and families at key developmental stages via a curriculum that uses elements of evidence-based programs and strategies to engage youth and caregivers. MEB Boxes have been tailored to meet different MEB needs across the life course. The Boxes will hold age-appropriate messages and information, personal treasures, and local resource contacts and will serve as an enduring, tangible reminder of the importance of MEB health. Each Box will include the program messages generated by the HPRN UPSTREAM! Advisory Council: 1) Mental, emotional, and behavioral health problems are common. Everybody in the community is affected; 2) MEB Problem is the new name, 3) MEB health problems can be prevented; 4) Prevention and early help are available in your MEB Box™; and 5) Get your MEB Box™ today! The MEB Box™ Program is a mechanism to focus community members’ attention, generate conversations about preventing MEB problems, and disseminate crucial messages for individuals and communities.
The MEB Box™ Program includes the MEB Baby Box™, which is disseminated through a local home visitation program; it provides parents with educational and support tools necessary for a thriving baby. MEB issues are common in adolescents, but even more common are the precursors in the years leading up to adolescence.7 The Tween MEB Box™ is a direct response to a detailed Northeast Colorado Child Health Care Capacity and Needs Assessment.8 This assessment identified resources that support child health and wellness in the region but also identified a lack of strong community culture supporting childhood health. The Tween MEB Box™ will provide every fifth-grade student with conversation tools, resilience tools, apparel, personal items for the child and parents, and local resources. The Tween MEB Box™ is delivered with a six-month curriculum that includes education around MEB and its prevention. Programs that facilitate parent-child communication have been shown to improve the quality of parent-child relationships and serve as protective factors to adverse problems, such as adolescent risky behaviors, poor academic achievement, and low self-esteem.9, 10 Since communication practices are modifiable behaviors,11 the curriculum will include tools, information, and interactive, evidence-based components for students, families, and teachers to develop practical strategies and communication skills for how to talk about MEB health. The curriculum will be delivered at “Get your MEB Box” events in partnership with schools.
Next steps for the MEB Box™ Program include the development of the Kinderbox MEB Box™, the Teen MEB Box™, and the Graduate MEB Box™ and curricula. HPRN is working closely with local agencies to anchor this MEB problem-prevention work in longstanding, local organizations serving their target population to ensure sustainability for years to come. The HPRN community-academic-clinical collaboration is poised to make a large and enduring difference in the health of Northeast Colorado.
Building Rural Communities of Solution
Rural communities do not have the same amount and types of resources that urban communities have. This means they do not have the same level of access to health care, behavioral health, and substance-use treatment as might be found in urban communities. However, rural communities have solutions and resourcefulness. With support from academic and philanthropic partners, they can build successful, evidence-based programs that are meaningful and locally relevant. Rural partnerships like the HPRN and its C.A.C. are successfully linking primary care, behavioral health, public health, and community organizations to build local communities of solution to address their local health needs. Rural community developers across the country can harness the wisdom and capacity of local communities of solution to help strengthen the mental, emotional, and behavioral health of individuals and families.
1. Colorado Department of Public Health and Environment, “Health Indicators.” Accessed July 2018.
2. Health Resources and Services Administration, U.S. Department of Health and Human Services, https://www.colorado.gov/pacific/cdphe/shortage-area-maps-and-data. Accessed July 2018.
3. National Commission on Community Health Resources (NCCHS), “Health Is a Community Affair.” Report (Cambridge, MA: Harvard University Press, 1966).
4. K.S. Griswold, S.E. Lesko, J.M. Westfall; Folsom Group, “Communities of Solution: Partnerships for Population Health,” Journal of the American Board of Family Medicine 26 (3) (May‒June 2013): 232‒38.
5. N. Norman et al., “Boot Camp Translation: A Method for Building a Community of Solution,” Journal of the American Board of Family Medicine 26 (2013): 254‒63.
6. J.M. Westfall et al., “Reinventing the Wheel of Medical Evidence: How the Boot Camp Translation Process Is Making Gains,” Health Affairs 35 (4) (2016).
7. K.R. Merikangas et al., “Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS‒A),” Journal of the American Academy of Child & Adolescent Psychiatry 49 (10) (2010): 980‒89.
8. J. Westfall et al., “Northeast Colorado Child Health Care Capacity and Needs Assessment.” Conducted for the Caring for Colorado Foundation (Denver, CO: Caring for Colorado Foundation, 2014).
9. V. Guilamo‐Ramos et al., “Parental Expertise, Trustworthiness, and Accessibility: Parent‐Adolescent Communication and Adolescent Risk Behavior,” Journal of Marriage and Family 68 (5) (2006): 1229‒46.
10. S.K. Riesch, L.S. Anderson, and H.A. Krueger, “Parent-Child Communication Processes: Preventing Children’s Health‐Risk Behavior,” Journal for Specialists in Pediatric Nursing 11 (1) (2006): 41‒56.
11. S.K. Riesch et al., “Effects of Communication Training on Parents and Young Adolescents,” Nursing Research 42 (1) (1993).


