Reposted with permission from the Robert Wood Johnson Foundation
In his now legendary approach to urban medicine, physician and Robert Wood Johnson Foundation grantee Jeffrey Brenner, MD, pioneered the technique of hot spotting—making block-by-block maps of Camden, N.J., examining residents’ hospital costs and identifying the handful of patients who cycled in and out of those institutions and racked up stratospheric medical bills.
What if America’s hospitals and health systems used similar techniques to identify the nation’s poorest and least healthy communities—and then teamed up with local community development organizations to set them on a path to better health?
David Fleming, a physician who directs Seattle’s public health department, made that pitch recently to members of the Foundation’s Commission to Build a Healthier America. National health reform, he said at the panel’s June 19 Washington meeting, affords an opportunity to nudge health care providers to reach outside their facilities to hot spot areas in need of health improvement. “The solutions to health in this country lie beyond the walls of the clinic and in our communities,” Fleming argued.
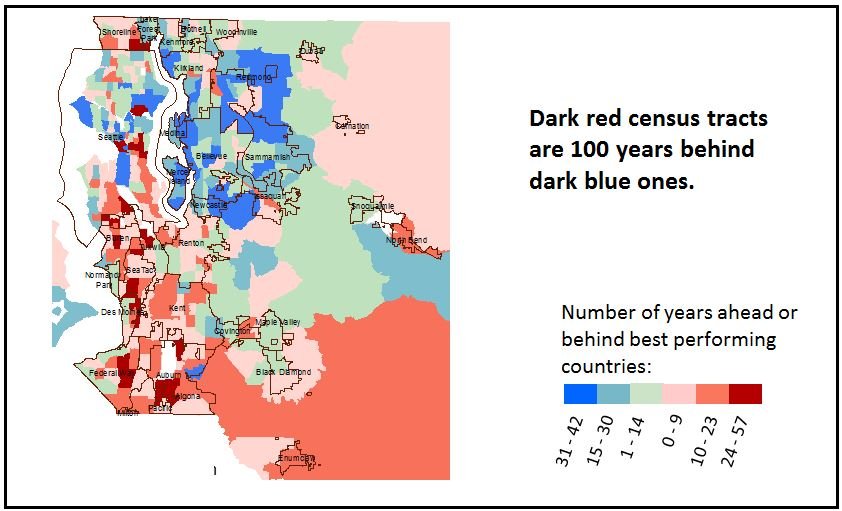
Offering an illustration, Fleming pointed to an analysis showing that some census tracts in King County, where Seattle is located, had average life expectancy that was years ahead of the 10 best-performing countries in the world—while others were lagging far behind (see illustration below).
King County life expectancy by census tract compared to average of top 10 countries, 2010
In Seattle and surrounding King County, Fleming said, public health authorities are helping hospitals and health systems hot spot these areas with the worst health indicators to encourage them to make a range of community-level investments. Fleming urged the commission to highlight provisions of the Affordable Care Act aimed at expanding hospitals’ and health systems’ role in population health. Specifically, the law requires the nation’s nonprofit hospitals to undertake a “community health needs assessment” every three years as a condition of retaining their federal tax-exempt status. Hospitals are also required to draft plans for addressing these local health needs.
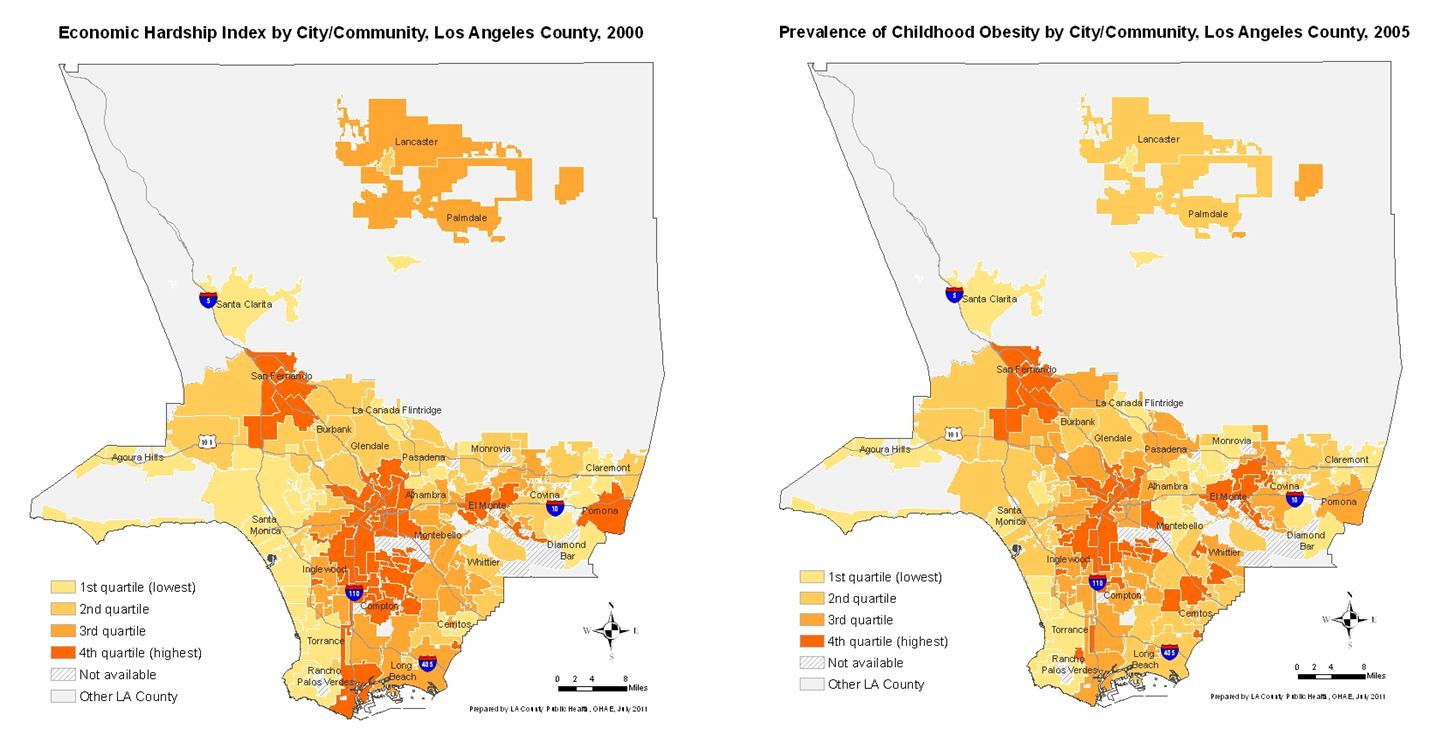
Similarly, David Erickson, director of the Center for Community Development Investments at the Federal Reserve Bank of San Francisco, showed the commission “heat maps” of Los Angeles County that demonstrated clear links between local communities’ economic circumstances and health. As he explained in his written testimony:
“The map on the left shows areas of economic hardship—a concern for community development—and the right map shows area prevalence of childhood obesity—a concern for public health. You can see that the maps are nearly identical. Today, [community development organizations, health-care providers and public health agencies] are working side-by-side in the same neighborhoods and often with the same residents, but we do not know each other or coordinate our efforts.”
Heat maps from the Los Angeles County Department of Public Health
Erickson pointed to examples of programs that had helped forge new avenues for improving health among health care providers, private-sector and philanthropic investors and community development organizations, as follows:
- The Healthy Futures Fund: The investment firm Morgan Stanley, the Kresge Foundation, and the New York-based Local Initiatives Support Corp. (LISC), a community development organization, teamed up to create a $100 million fund that finances health clinics and affordable housing. The clinics can obtain below market-rate financing if they can demonstrate that beyond providing health care, they also address the broader social determinants of health.
- ReFresh: To address the problem of “food deserts” in New Orleans, Goldman Sachs and JP Morgan-Chase are financing construction of this “Healthy Food Hub” in the Mid-City neighborhood. On a site once left vacant by Hurricane Katrina, a Whole Foods will offer lower-than-normal prices for local residents; a local charter school will have a new home; and in a state-of-the-art teaching kitchen, Tulane medical students, physicians and members of the community will learn healthful cooking.
- The Bay Area Transit-Oriented Affordable Housing Fund: Several investment firms and community development financial institutions teamed up to provide $50 million to develop mixed-income housing and walkable neighborhoods near San Francisco. The development is to be located near public transit, whose proximity will both increase residents’ physical activity and connect them to jobs elsewhere in the area.
The clear message to the commission is that advancing a community’s health is everybody’s business—not just that of health care providers or public health agencies. “We’re not thinking in silos anymore,” said Laura Trudeau, senior program director for community development at the Kresge Foundation. “All of us are working across every boundary that we can break.”
The views expressed here do not necessarily reflect the views of the management of the Federal Reserve Bank of San Francisco or of the Board of Governors of the Federal Reserve System.