Many regions around the world are at increased risk of changing environmental conditions, such as water shortages, extreme temperatures, natural disasters, floods, droughts, and rising sea-levels.1 These events are increasing in severity and frequency. As these global trends unfold, countries must also grapple with an aging populace. People are living longer than ever before and societies are increasingly dealing with the novel challenge of supporting remarkably large numbers of older citizens and denizens.2 Climate change and shifting demographic patterns require innovative ideas about how to build and adapt community infrastructure that helps older individuals thrive. Urban planners, and community investors will need to consider aging populations as they think about how the built environment can promote healthy local communities in the face of a changing climate that has acute and unique consequences for individuals aged 65 and over.
In this article, we briefly review: (i) global aging patterns; (ii) the connection between climate change and the health of older-age people; and (iii) a conceptual model that planners and community leaders may use to move forward. Ensuring global healthy aging requires community development solutions that address the direct health risks and the social costs of being older-aged during a time of climate change.
An Aging Population
The increase in older individuals across the world is a direct result of demographic changes such as the transition from high to low birth and death rates. The average decrease in global fertility rates means that recent birth cohorts are smaller in size than before. Increases in life expectancy translate into larger populations of older individuals. Taken together, these trends result in a higher proportion of middle and older individuals in a given country’s population.3 In the U.S., for instance, one in five people will be 65 or older by the 2030. 4 This aging trend is common in high-income countries such as Japan, the U.S., and Australia.5 For some low- and middle-income countries, however, the drastic shift in population age structure has yet to come.
Societies cannot ignore how aging warrants the attention of many concerned with the link between the built environment and the wellbeing of communities. People are living longer than before, and the years of life gained over the past decades in life expectancy are often lived in unhealthy and physically limited conditions.6 The Centers for Disease Control and Prevention estimates that 80 percent of older adults (aged 60 and over) are experiencing at least one chronic disease such as cardiovascular disease, cancer, cognitive decline, and/or diabetes.7 These are current issues that aging populations face. Now, when climate change and extreme weathers events are included in the discussion of older-age wellbeing, community-level solutions are required.
Climate Change and Health Risks
Global climate change increases individuals’ susceptibility to adverse health conditions. Temperature extremes and increased natural disasters such as hurricanes, wildfires, and droughts all contribute to the health of people and communities.8 Climate change places disproportionate stress on individuals with already vulnerable health status, notably aging adults. Older adults struggle with physical mobility and often live with one or more chronic health condition.9 Extreme temperature events can exacerbate chronic health conditions and places older adults at risk for increased health care and social services utilization.10 Furthermore, the evacuation of older adults prior to, during, and after natural disasters poses extreme logistical issues, particularly if they are living alone, or in long-term care facilities.11 This can further reduce their access to services and can worsen stress-related health conditions.12
Physical and social environments have a direct impact on health. Climate change directly influences human health and disease by destabilizing core infrastructure necessary for community health. Using severe droughts as one example, vulnerable communities may lack core natural food and water resources. In the global context, developing countries struggle in situations of drought. Migration is often one short-term solution for afflicted communities. However, migration is difficult for older adults. Thus, droughts and extreme temperatures require adequate shelter and transportation. The absence of infrastructure that considers the needs of older adults in climate-driven crisis threatens more than a comfortable lifestyle—it undermines basic access to health care, food, and other living necessities.13
Climate-change-induced conditions influence the health of older-aged communities in a dynamic way because it not only directly increases their health risk, but also affects their social lives. One third of the older non-institutionalized population lives alone. People who are older and who live alone may be at increased risk during climate change events because of their potential for being physically limited, having multi-morbidities, and being at increased risk of hospitalization.14 People who are poor and do not have the resources to move post-natural disaster will also be critically and disproportionately impacted.
Why Community Development Matters for Aging and Climate Change
Community-based interventions that consider aging and climate change issues can improve quality of life and prevent unnecessary costs for communities. One promising intervention avenue is to build or adapt community infrastructure in ways that support healthy lifestyles among older adults. For instance, increasing the number of parks, grocery stores, and health clinics in neighborhoods where older adults live relaxes the burden of physical mobility constraints. Improvement of transportation systems ensures adequate space for older adults and people with disabilities. These kinds of investments are necessary not only to promote the general health of aging individuals, but also to address some of the risks associated (in response to increased heat-waves, for instance) with climate change, which hurt the aging population the most. These interventions have the potential for high returns. In examining the relationship between living in a walkable neighborhood and mortality risk among older adults, researchers found that those who lived in more walkable spaces had higher chances of survival in older age.15
The ability to relocate in response to climate change is driven by many factors, including financial security, social networks, and physical mobility. Low-income older-aged individuals face a double jeopardy of disadvantage that hinders their capacity to survive the effects of climate change. Second, the community infrastructure of neighborhoods with evidently less investment may experience more damage. This means that local community developers who care about aging and climate change infrastructure need to consider additional factors. Different contexts (e.g., rural vs. urban, low vs. high-income countries) require different strategies.16
Adaptation strategies include the diversification of assets, such that households do not only rely on one kind of crop or business for economic survival.17 For instance, farmers in rural places and in unstable places can diversify the technologies of their crops, and/or learn new trades to supplement their livelihoods. However, even the extent of participation in adaptation strategies to climate change varies by age. For example, a study of farmers in Eastern Kenya found that older farmers are less likely to uptake new technologies and grains that would mitigate the impact of droughts on their product.18 This is a perfect example of how development interventions about climate change need to consider aging populations and how to help support them as they cope with climate-induced changes and disasters.
One potent solution is inter-sectoral collaborations. Public health departments should collaborate with urban planners to create accessible apartments for older people. Updated building codes could require backup generators to support possible power outages during extreme weather events. Urban planners should find ways to promote the social lives of older people because social connectedness can uplift the mental health of older people and serve a practical purpose. Public-private partnerships are especially important to consider because they combine funding mechanisms to promote both healthy investments and social infrastructure in local communities. One example of a possible public-private partnership would be a housing development funded by private investors but supported by public subsidies for older people who cannot otherwise afford to live there.
Our team developed a Model for Healthy Aging for practitioners that guides an understanding of the climate-change-induced health risks of the elderly population. The model shows how developers, health experts, planners, and community leaders can address this issue. The model assigns a climate change event to the risk it poses for the elderly and provides a potential area of investment to address that risk. Below, we review the main tenets of the model and supplement these key points with relevant empirical literature:
Improve mobility/transportation systems that increase accessibility for older individuals. Urban planning and design can strengthen cities and communities with public spaces that are accessible and that carry potential to promote social connectedness.19 Mobility also means migration. In regions with rising waters and flooding, one of the strategies of adaptation is retreating from the space, encouraged by buyouts. These buyouts need to be financed and they often are funded by the state or entities like the U.S. Federal Emergency Management Agency (FEMA). More people need them than receive them, which “condemns some to live through multiple disasters.”20
Promote affordable community living and community-supported solutions to social isolation. Older people rely on several forms and sources of housing. Housing options include subsidized housing with associated programs that ease health care access. However, these housing projects are limited in number and should be expanded.21 Older people who live with others adapt better after natural disasters.22
Support access to creative health care provision, such as mobile clinics/teams. Tackling health issues in underserved communities can lead to not only community-wide health improvements but also significant cost savings. Mobile health clinics, for example, improve access to health care while also overcoming negative social determinants of health.23 This cost-effective care delivery model should be more readily considered as a solution to address the needs of the elderly population and should be integrated into health care systems more frequently.
Improve housing infrastructure, including access to air conditioning and power back-up options. There are promising technological advancements to improve how we think about places and aging. For instance, gaming technology has been used to plan infrastructure and housing projects to facilitate designer and client housing prototypes using digital design.24 These designs can be used to produce prototypes of living spaces that are responsive to both climate change and aging needs.
Create access to green spaces. In Taiwan, increasing access to green spaces has improved the health of the elderly.25 Community environments support physical activity and social connections for the elderly. This intervention revealed that when available, older adults not only accessed the spaces but also asked for a combination of structured activities and age appropriate physical exercises. Thus, evidence reveals that green spaces are a viable intervention to improve the health of older adults.
Figure 1
The Model for Healthy Aging that bridges climate, change, health, and community development needs
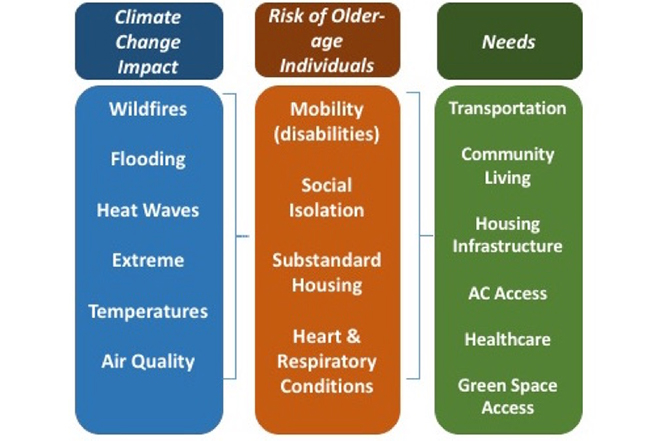
Figure 1 is the conceptual Model for Healthy Aging, which ties together the health-climate change link and the global aging phenomenon. The model shows that increasing the resources in the physical and social environment are important building blocks that can help mitigate the adverse community health effects of the aforementioned climate change events. Efforts to increase infrastructure for climate change adaptation for the aging community need to work across more than one of these community resources.
Our model builds on the four action areas of the Robert Wood Johnson Foundation’s Culture of Health Framework.26 The framework is a movement that promotes cross-sector collaboration to strengthen systems that would, in turn, create healthy and equitable communities.27 It depicts a movement in thought and practice that allows stakeholders from all fields to join forces to improve people’s health. The built environment is directly associated with health outcomes.28 In the face of changing climate conditions and increased prevalence of extreme weather events, the built environment needs to transform in order to meet the health needs of the most vulnerable populations.
Community development practitioners should consider investing in projects that address the wellbeing of the community as a whole. Investment in infrastructure will have ripple effects not just for the health of the elderly but those with disabilities and other vulnerable populations. Improved infrastructure and healthier elderly populations will decrease costs to health care systems, which can lead to a reinvestment of savings in other public goods. An investment in health is an investment in all of society.
Practical Recommendations and Implications
In addition to a conceptual framework, there are practical recommendations for current and long-term projects. First, the language of contracts in development projects that aim to increase equity need to include a memorandum of understanding for vulnerable populations. Specific language in the contract will assure access for those living in poverty. Investors and planners who seek to create affordable solutions should ensure that new projects do not increase inequities in the aging community. Second, developers and planners can use our Model for Healthy Aging to account for the top three needs for the community of interest: transportation, housing, and health care. Third, development projects that promote healthy aging in the face of climate change need to be sustainable. To ensure the success of community development projects after their creation, they need to have a responsible and prepared leadership team at the helm. Teams should be equipped with the financial knowledge that will ensure stability and sustainability.
Looking forward, we need to examine the models of sustainable aging pioneered by other countries. The following are structural changes that would ensure a safer future for elderly populations:
- Policy development: ensure sustainable public finances to guarantee adequate pensions, health care, and long-term care.
- Reform current health care systems: ensure adequate systems of long-term care exist to ensure wellness.
- Human capital development and inclusive growth: support economic and social integration by setting up systems that allows volunteer and job opportunities.
- Intergenerational perspective: create social awareness that we are all aging individuals, to help those who are currently in the latter stage of life, ensuring a safer future for us all.
This last point is critical because public engagement and awareness is one of the most important aspects of social and community change. Average individuals who may not think or perceive that climate change threatens their livelihoods need to be included in conversations in order to have a wider net of allies and supporters for healthy aging infrastructure.29 Collective action will increase intentional dialogue about the issues and solutions that these conversations need.
Conclusion
The changing demographic landscape prompts developers and planners to consider the needs of aging individuals. The built environment is an opportunity for meaningful intervention. Aging populations not only require novel and health-promoting built environments, but also a shift in the priorities of developers and investors. Currently, aging is at the margins of conversations about both climate change and community development. In order to age with dignity, we should insist on an integration of community development, environmental science, and health.
1. Kousky, C. “Informing climate adaptation: A review of the economic costs of natural disasters,” Energy Economics, 46 (2014), pp. 576-592; Trenberth, K.E. et al. “Hurricane Harvey links to Ocean Heat Content and Climate Change Adaptation,” Earth’s Future (2018).
2. Riley, J.C. “Estimates of regional and global life expectancy, 1800–2001,” Population and Development Review, 31(3) (2005), pp. 537-543.
3. Pantazis, A. and Clark, S.J. “A parsimonious characterization of change in global age-specific and total fertility rates,” PLoS ONE, 13(1), e0190574 (2018); Stolnitz, G.J. “The demographic transition: from high to low birth rates and death rates,” Population Growth (2017), pp. 30-46.
4. United States Census Bureau. “Older People Projected to Outnumber Children for First Time in U.S. History” (2018).
5. Lee, R.D. “Demographic change, welfare, and intergenerational transfers: a global overview,” Ages, Generations and the Social Contract (2007).
6. Crimmins, E.M. and Beltrán-Sánchez, H. “Mortality and morbidity trends: is there compression of morbidity?” The Journals of Gerontology: Series B, 66(1) (2011), pp. 75-86.
7. Centers for Disease Control Prevention and Merck Company Foundation. “The State of Aging and Health in America 2007” (2007).
8. Gamble, J.L. et al. “Climate change and older Americans: state of the science,” Environmental Health Perspectives, 121(1) (2012), pp. 15-22; Geller, A.M. and Zenick, H. “Aging and the environment: a research framework,” Environmental Health Perspectives, 113(9) (2005), p. 1257.
9. Kriegsman, D.M., Deeg, D.J., and Stalman, W.A. “Comorbidity of somatic chronic diseases and decline in physical functioning: the Longitudinal Aging Study Amsterdam,” Journal of Clinical Epidemiology, 57(1) (2004), pp. 55-65.
10. Geller, A.M. and Zenick, H. “Aging and the environment” (2005); Gronlund, C.J. et al. “Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006,” Environmental Health Perspectives, 122(11) (2014), p. 1187.
11. Gamble, J.L. et al. “Climate change and older Americans” (2012).
12. Rosenkoetter, M.M. et al. “Perceptions of older adults regarding evacuation in the event of a natural disaster,” Public Health Nursing, 24(2) (2007), pp. 160-168.
13. Martin, S.A. “A framework to understand the relationship between social factors that reduce resilience in cities: application to the City of Boston,” International Journal of Disaster Risk Reduction, 12 (2015), pp. 53-80; Kiyota, E. “Co-creating Environments: Empowering Elders and Strengthening Communities through Design. What Makes a Good Life in Late Life? Citizenship and Justice in Aging Societies,” Hastings Center Report, 48(5) (2018), S46-S49; Greenfield, E.A. “Age-Friendly Initiatives, Social Inequalities, and Spatial Justice,” Hastings Center Report, 48(5) (2018), S41-S45.
14. Legrand, D. et al. “Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old,” Journal of the American Geriatrics Society, 62(6) (2014), pp. 1030-1038.
15. Takano, T., Nakamura, K., and Watanabe, M. “Urban residential environments and senior citizens’ longevity in megacity areas: the importance of walkable green spaces,” Journal of Epidemiology & Community Health, 56(12) (2002), pp. 913-918.
16. Agrawal, A. “The role of local institutions in adaptation to climate change,” World Bank (2008).
17. Lin, B.B. “Resilience in agriculture through crop diversification: adaptive management for environmental change,” BioScience, 61(3) (2011), pp. 183-193.
18. Mugi-Ngenga, E. et al. “Household’s socio-economic factors influencing the level of adaptation to climate variability in the dry zones of Eastern Kenya,” Journal of Rural Studies, 43 (2016), pp. 49-60.
19. Schuur, S. “Designing for Future Uncertainties: Comparative Studies of Two Adaptive Strategies in Urban Design in New York and Sweden,” Climate Change Adaptation in North America (Leal, W. and Keenan, J.M. [eds.]) (2017), pp. 177-191.
20. Wiseman, R.F. “Why older people move” (1980).
21. Gibler, K. “Aging subsidized housing residents: A growing problem in US cities,” Journal of Real Estate Research, 25(4) (2003), pp. 395-420.
22. Kwan, C. and Walsh, C.A. “Seniors’ disaster resilience: a scoping review of the literature,” International Journal of Disaster Risk Reduction, 25 (2017), pp. 259-273.
23. Stephanie, W. et al. “The scope and impact of mobile health clinics in the United States: a literature review,” International Journal for Equity in Health, 16(1) (2017), p. 178.
24. Wu, W. and Kaushik, I. “Design for sustainable aging: improving design communication through building information modeling and game engine integration, Procedia Engineering, (118) (2015), pp. 926-933.
25. Pleson, E. et al. “Understanding older adults’ usage of community green spaces in Taipei, Taiwan,” International Journal of Environmental Research and Public Health, 11(2) (2014), pp. 1444-1464.
26. Robert Wood Johnson Foundation. “Building a Culture of Health: An Action Framework,” Vision to Action: Measures to Mobilize a Culture of Health Report (2016).
27. Mockenhaupt, R. and Woodrum, A. “Developing evidence for structural approaches to build a culture of health: A perspective from the Robert Wood Johnson Foundation,” Health Education & Behavior, 42(1_suppl) (2015), 15S-19S.
28. Berrigan, D. and McKinno, R.A. “Built environment and health,” Preventive Medicine, 47(3) (2008), p. 239.
29. Myers, C.D., Ritter, T., and Rockway, A. “Community Deliberation to Build Local Capacity for Climate Change Adaptation: The Rural Climate Dialogues Program,” Climate Change Adaptation in North America (Leal, W. and Keenan, J.M. [eds.]) (2017), pp. 9-26.